In the shadowy realm of silent health threats, a viral culprit is steadily reshaping the landscape of cancer risk, targeting an unsuspecting demographic with increasing precision. Human Papillomavirus (HPV), once considered a peripheral health concern, has emerged as a potent harbinger of malignancy, casting its long, ominous shadow over a specific population group. As medical researchers unravel the intricate patterns of transmission and susceptibility, a disturbing trend is coming into sharp focus: HPV-linked cancers are no longer a distant possibility but a growing reality for a particular segment of society. This article delves into the complex interplay of biology, behavior, and risk factors that are propelling this concerning health phenomenon, offering a clear-eyed examination of who stands at the greatest vulnerability in this unfolding medical narrative. Recent studies have revealed a concerning trend in cancer diagnoses, highlighting a important increase in HPV-related malignancies among a specific demographic. Oropharyngeal squamous cell carcinoma, primarily affecting the back of the throat, has been steadily rising, with human papillomavirus playing a critical role in its advancement.
Men in their 40s and 50s are experiencing the most considerable surge in these cancer cases.Researchers attribute this trend to complex sexual behavior patterns and changing viral transmission dynamics. Unlike previous generations, individuals in this age group have experienced diverse sexual experiences during periods with less extensive HPV vaccination programs.
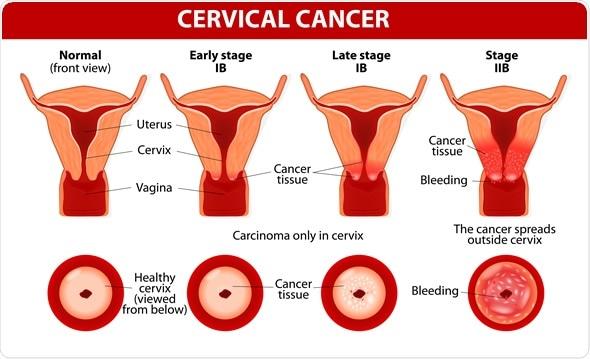
The virus, traditionally associated with cervical cancer, has demonstrated remarkable adaptability in targeting multiple anatomical regions. Oral and throat cancers linked to HPV have become particularly prevalent, challenging conventional understanding of viral transmission and cancer progression.
Medical professionals emphasize that sexual history significantly influences risk factors. Multiple lifetime partners,inconsistent protection,and specific intimate practices contribute to increased viral exposure. The complex interplay between viral strain, immune response, and individual genetic predispositions creates a nuanced landscape of potential infection and subsequent malignancy.Vaccination strategies have emerged as a pivotal intervention. Recommended for individuals between 9 and 45 years old, these immunological safeguards provide substantial protection against high-risk HPV strains. However, existing populations who missed early vaccination windows remain particularly vulnerable.
Diagnostic challenges persist, with many cases remaining asymptomatic during initial stages. Subtle symptoms like persistent throat discomfort, unexplained weight loss, and difficulty swallowing can signal potential malignant change. Early detection remains crucial for successful treatment outcomes.
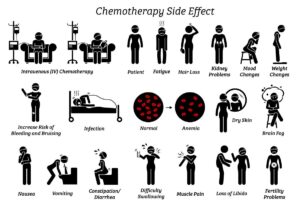
Emerging research suggests lifestyle factors also play a significant role. Smoking, alcohol consumption, and compromised immune systems can exponentially increase susceptibility to HPV-related cancers. Holistic prevention approaches encompass not just vaccination but comprehensive health management.
Genetic screening and personalized risk assessments are becoming increasingly sophisticated. Advanced diagnostic technologies enable more precise identification of high-risk individuals,allowing targeted interventions and monitoring.
Healthcare systems worldwide are adapting their screening protocols to address this evolving epidemiological landscape. Interdisciplinary approaches combining virology,oncology,and public health strategies are essential in mitigating potential cancer risks.
Despite growing awareness, significant knowledge gaps remain. Continued research, public education, and proactive healthcare strategies will be instrumental in reducing HPV-related cancer incidences and improving overall population health outcomes.