In the labyrinth of over-the-counter cold remedies, a bombshell revelation has emerged from the hallowed halls of the FDA: a common decongestant ingredient may be nothing more than a pharmaceutical placebo. As millions of sniffling, congested Americans reach for their trusted cold medicines, a critical question hangs in the air like a stubborn winter fog: If this go-to ingredient is ineffective, what truly offers relief when the sneezes and stuffiness strike? This investigation peels back the layers of pharmaceutical claims, scientific scrutiny, and potential alternative treatments that might actually clear your airways and bring some much-needed comfort during cold and flu season. The recent bombshell from the Food and Drug Administration has sent shockwaves through the over-the-counter cold medicine industry. Phenylephrine, a staple decongestant found in countless medications lining pharmacy shelves, has been officially declared ineffective when taken orally.
For decades, consumers have trusted brands like Sudafed PE and Mucinex, believing these medications would provide relief from nasal congestion. Clinical studies now reveal these products offer no significant improvement over placebos, leaving millions wondering about alternative strategies for combating stuffy noses.
Natural remedies emerge as powerful contenders in the congestion-fighting arena. Saline nasal sprays provide immediate relief by moisturizing and clearing nasal passages without chemical interventions. Hydration plays a crucial role, with warm liquids like herbal tea and broths helping thin mucus and reduce inflammation.
Nasal irrigation techniques, such as neti pots, offer remarkable congestion relief. These tools flush out irritants and mucus, providing substantial breathing improvements. Steam inhalation remains another time-tested method, helping to loosen mucus and open respiratory pathways.
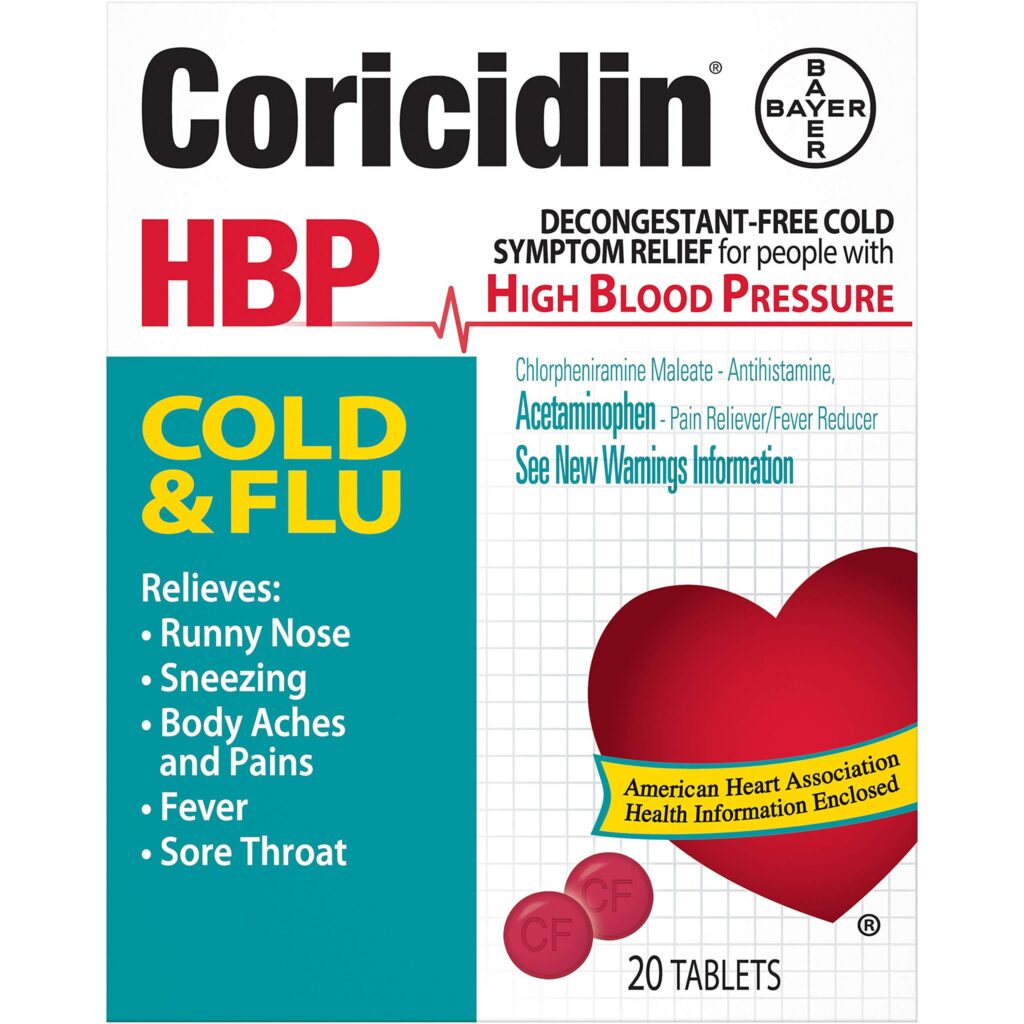
Pharmaceutical alternatives still exist. Pseudoephedrine, available behind pharmacy counters, continues to demonstrate effectiveness. Patients must present identification and sign documentation due to potential misuse in methamphetamine production, but the medication remains a legitimate decongestant option.
Prescription nasal corticosteroid sprays represent another scientifically validated approach. Medications like fluticasone and mometasone reduce nasal inflammation directly, offering targeted relief without systemic side effects.
Lifestyle modifications can significantly impact congestion management. Adequate sleep, balanced nutrition, and stress reduction support immune function and respiratory health. Regular exercise improves overall circulation and respiratory efficiency.
Humidifiers introduce moisture into living spaces, preventing nasal passage dryness and reducing congestion potential. Essential oils like eucalyptus and peppermint can provide additional respiratory support when diffused or applied topically.
Zinc supplements and vitamin C demonstrate potential in reducing cold symptom duration and severity. Emerging research suggests these nutritional interventions might help the body combat respiratory infections more effectively.
Consulting healthcare professionals remains critical. Individual health conditions, allergies, and potential drug interactions require personalized medical guidance. While over-the-counter options may seem convenient, professional advice ensures safe and effective treatment.
The FDA’s announcement doesn’t signify a complete elimination of decongestant options but rather encourages consumers to explore more scientifically substantiated approaches to managing respiratory discomfort.