Numbers don’t lie, they say—but what if they’re telling the wrong story? For decades, Body Mass Index (BMI) has been the go-to metric for determining health, plastered across medical charts and fitness websites like an unquestioned gospel. Yet, beneath its seemingly simple calculation lies a measurement riddled with flaws, oversimplifying the complex narrative of human bodies and wellness. This article peels back the layers of the BMI myth, challenging a standard that has long masqueraded as scientific truth, and explores more nuanced, accurate alternatives that truly reflect individual health. For decades, the Body Mass Index (BMI) has been the go-to metric for determining health and weight status. But what if this widely accepted measurement is fundamentally flawed? Scientists and health professionals are increasingly questioning its validity, revealing a method that’s more pseudoscience than precision.
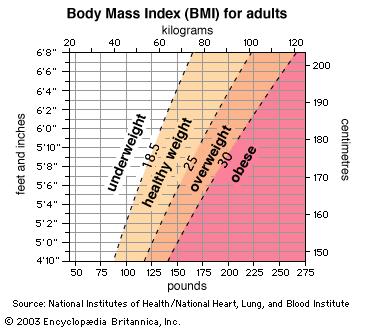
Originally developed in the 1830s by mathematician Lambert Adolphe Jacques Quetelet, BMI was never intended to be a health diagnostic tool. It simply divides a person’s weight by their height squared, creating a numerical category that supposedly indicates health risks. However, this simplistic calculation fails to account for crucial factors like muscle mass, bone density, overall body composition, and individual physiological differences.
Athletes and muscular individuals often register as “overweight” or “obese” despite being incredibly fit. Conversely, someone with a “normal” BMI could have dangerous metabolic issues hidden beneath a seemingly healthy exterior. This one-size-fits-all approach ignores the complex reality of human bodies.
Modern healthcare demands more nuanced assessments. Waist-to-hip ratio emerges as a more reliable indicator of potential health risks. This measurement considers fat distribution, particularly dangerous visceral fat surrounding internal organs. Research consistently shows that abdominal fat correlates more directly with cardiovascular diseases and metabolic disorders than overall weight.
Another promising alternative is body fat percentage. Advanced techniques like DEXA scans and hydrostatic weighing provide precise measurements of body composition. These methods distinguish between muscle, fat, and bone, offering a comprehensive health snapshot that BMI cannot match.
Metabolic markers offer another critical perspective. Blood tests measuring cholesterol, insulin resistance, inflammation levels, and hormone balance provide insights far beyond a simple height-weight calculation. These comprehensive assessments reveal underlying health conditions that BMI completely overlooks.
Genetic testing and personalized metabolic screenings represent the future of health assessment. By understanding individual genetic predispositions and metabolic functioning, healthcare professionals can develop truly personalized wellness strategies.
Physical fitness tests also provide meaningful health indicators. Measuring cardiovascular endurance, strength, flexibility, and recovery rates gives a holistic view of an individual’s physical condition that no single numerical index can capture.
The medical community’s gradual shift away from BMI reflects a broader understanding that health is multifaceted. No single measurement can encapsulate an individual’s overall wellness. Comprehensive, personalized assessments considering multiple factors are essential for accurate health evaluations.
As research advances, we’re moving towards more sophisticated, nuanced approaches that respect human biological diversity and complexity.